“PBM” Reform and Defending Patient Access
PBM Reform as Must-Pass Legislation
71% of registered voters agree that Congress should consider legislation to reform pharmacy benefit managers’ role and actions in healthcare to be a top priority in 2025.
PBM Reform as Must-Pass Legislation
71% of registered voters agree that Congress should consider legislation to reform pharmacy benefit managers’ role and actions in healthcare to be a top priority in 2025.
This poll was conducted by Morning Consult and commissioned by NACDS between October 1-October 3, 2024, among a sample of 1,778 Registered Voters. The interviews were conducted online and the data were weighted to approximate a target sample of Registered Voters based on gender by age, educational attainment, race, marital status, home ownership, race by educational attainment, 2020 presidential vote, and region. Results from the full survey have a margin of error of plus or minus 2 percentage points.
To Reduce Americans’ Drug Costs and Protect Pharmacy Access, All Levels and Branches of Government Must Act
The complexities of the issues make it necessary for the federal and state governments to do their part to bring about comprehensive PBM reform. Only if the federal and state governments do their respective parts will reform prevent “pharmaceutical benefit manipulation” across all markets – Medicare, Medicaid, and commercial.
For All In Government
Stop Manipulation of Drug Prices, Medication Access, & Pharmacy Freedom
Estimates project that PBMs more than doubled their revenue over the course of the last decade and will do so again in the current decade. For example, Fortune Business Insights projects PBM revenues of more than $800 billion by 2030, and Grand View Research projects more than $900 billion. See how they do it at the expense of patients, pharmacies, and others. And how to fix it.
PBM reform is vital for patients and pharmacies.
These are essential principles for comprehensive PBM reform – to help stop PBMs’ manipulation and to stand up for patients’ pharmacy access and for pharmacies’ survival:
For the U.S. Congress
Real PBM Reform Must Protect Americans on Medicare and Medicaid, and Their Pharmacies
Call the Vote on PBM Reform
“Time Is Now” Ad
July 2024 Congressional Hearing
March 2024 Press Conference
“Get It Done” Ad
“Real Reform” Ad
For all Americans and for the pharmacies serving them, it is essential for the 119th Congress to finally enact PBM reforms. Throughout the 118th Congress, bipartisan leaders in Congress achieved consensus on needed reforms supported by NACDS. Unfortunately, the 118th Congress didn’t finish the job. The hard work already has been done to recognize the problems caused by PBM practices and to craft and agree on meaningful and sound policies that now must be enacted without delay.
Congressional consensus includes vital reforms in Medicare, Medicaid, and the commercial markets – which have been developed by the Senate Finance Committee; the Senate Health, Education, Labor, and Pensions Committee; the House Energy and Commerce Committee; and the House Ways and Means Committee. Importantly, other committees like the House Oversight and Accountability Committee and the Senate Judiciary Committee have contributed valuably through oversight hearings and investigations into PBM tactics.
The consensus includes Medicare and Medicaid reforms contained in legislation that advanced in the 118th Congress, including the Modernizing and Ensuring PBM Accountability Act (S. 2973); the Better Mental Health Care, Lower-Cost Drugs, and Extenders Act (S. 3430); and the Lower Costs, More Transparency Act (H.R. 5378). The consensus also includes certain commercial market reforms included in the Pharmacy Benefit Manager Reform Act (S. 1339).
To be clear, NACDS and pharmacy coalition partners emphasize that the first step toward real reform must include:
- Medicaid managed care pharmacy payment reform and a ban on spread pricing;
- Defining and enforcing reasonable and relevant Medicare Part D pharmacy contract terms;
- Establishing relevant, standardized and transparent pharmacy quality measurements in Medicare Part D.
For the States
Bipartisan Focus is Producing Results Across the Nation
States are recognizing the need to enact PBM reform – and to press forward with implementation, enforcement, and oversight despite PBMs’ efforts to roll back reforms. From 2021 to 2023, states have enacted more than 130 new PBM reform laws. One or more aspects of the NACDS Principles of PBM Reform now have been adopted in every state – though much, much more work is needed in the states. Further, this does not in any way mitigate the need for federal action on the issues that it must address.
State Spotlight:
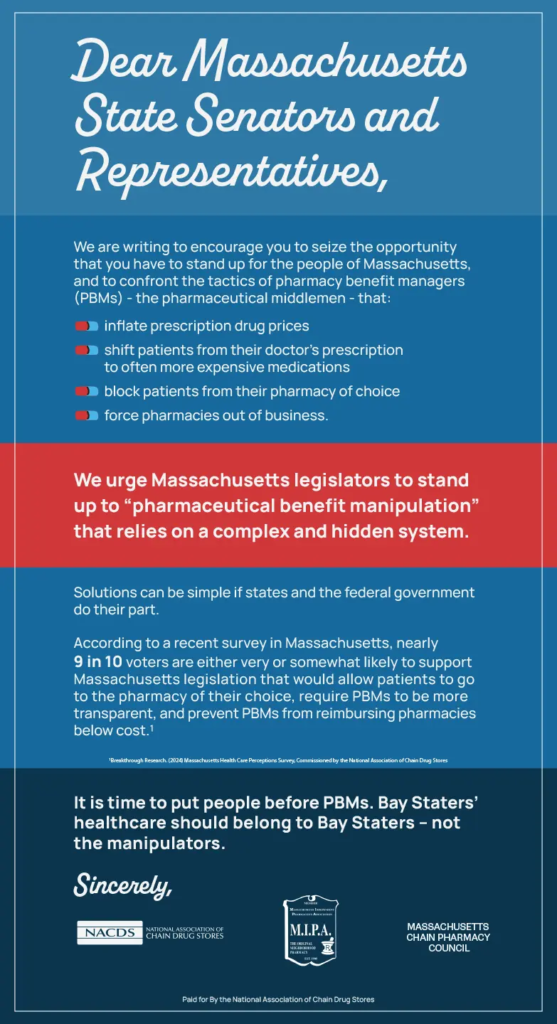
NACDS Urges Massachusetts to Proceed with Much-Needed PBM Reform Legislation
Massachusetts “Get It Done” Ad
Massachusetts PBM Reform Explainer Ad
Massachusetts “Stand Up” Radio Ad
Massachusetts Voters Want PBM Reform
A newly released survey reveals that Massachusetts voters are tired of rising healthcare costs and are looking to PBM reform for much-needed relief.